Delta Dental Insurance
Provider Recredentialing
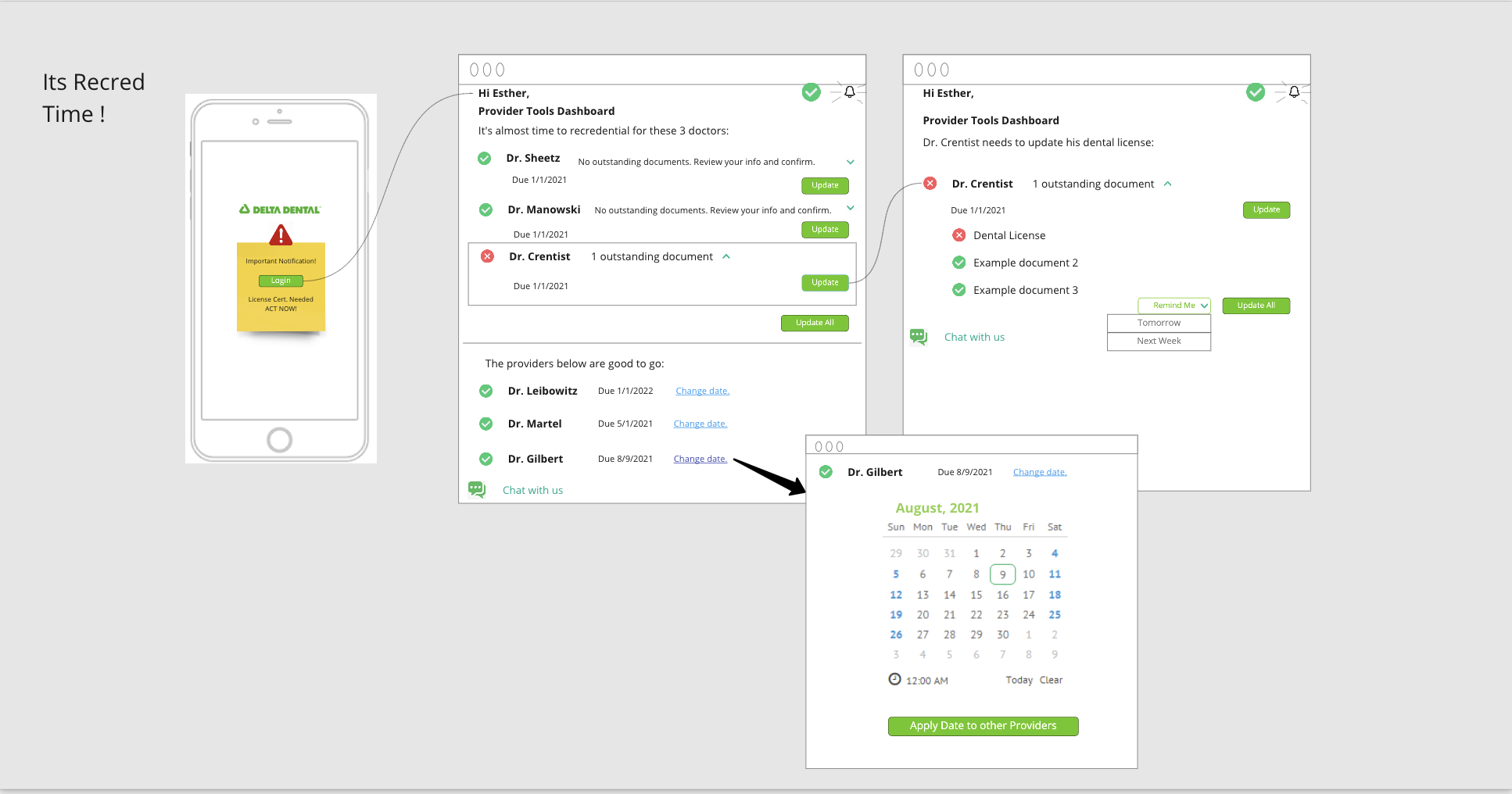
Transitioning from paper mail alerts and paper forms to email notifications, status update alerts, dashboard and digital form.
My role
Design Lead / Lead Product Designer, responsible for email notifications and alerts and status dashboard.
Project summary
There is a need for Delta Dental Providers to recredential to provide proof that their qualifications are still current and valid. Creating a digital recredentialing experience is a means to enhance recredentialing, so that Providers have a more simplified and streamlined process.
Currently, the paper-based process has limitations and creates friction. Some of these pain points include a lack of communication and visibility into the status of the process. Paper mail campaigns for Providers with multiple offices, multiple insurance plans and multiple practices in one office, can often create confusion as to how to start, and which step should go first. When they are first notified, Providers who start the process early, still have to wait for approval and completion of the process. This is due to a queue order that is based on date of expiration rather than real-time processing. The goal of the project was to create a digital experience to solve these problems.
User research gathered through surveys and 1-on-1 interviews showed us that there was an inherent problem with recredentialing. We found that the process of recredentialing should be a simpler one. Delta Dental sends a reminder letter; the Provider completes and sends in paperwork; and, Delta Dental processes the paperwork and recredentialing is complete. Each step in the process however, involved pain points and friction in real life usage.
When Delta Dental sends the reminder letter, it's sent out at 6 months prior to expiration as well as 3 months prior, and an ominous final notice is sent out 1 month prior to credential cancelation.- We found that repeated notification letters caused over half the participants to re-do & re-send paperwork even when they didn’t have to.
- There was confusion over the "ownership" of the recredentialing process in practices that have multiple offices.
- Completing and sending in the paperwork in a timely fashion was not rewarded with a quicker completion. Paperwork was processed in an order of credential expiration date, rather than first come, first served. Since this is not communicated, it tends to lead to a feeling of learned helplessness.
- There is a feeling of wasted time when paperwork goes back-and-forth when errors occur.
- Providers don't always know if and when Delta Dental received the paperwork because there is no feedback or confirmation given.
- Some Providers think it's a waste of time, having other things to do.
- It's not difficult, but you do have to pay attention to the forms and what you're filling out since there are often times more than 1 Provider in a Practice.
- With many licenses, numbers, and DEA numbers that all need to match up, it's easy to make a mistake, making it time consuming when the data needs to be corrected.
- Providers wish it were easier to recredential than the first time around you do it, it ends up being the same process over and over again.
- Previous information is not carried over to the new recredentialing form. Many times information is has not changed and Providers wish they would just look over the information and confirm that information is current, rather than filling out and re-entering data.
- Providers found that the lack of alerts or any information regarding the approval left them feeling in the dark.
- Providers didn't feel confident in the process, and it left them feeling the need to call Delta Dental, spending sometimes, hours on the phone for information that was missing or needed to be verified.
- Overall, Providers wanted to reduce the need to be on the phone and more specifically, be on hold. Mentioning the usefulness of a chat feature that would allow for multitasking and passively getting the job done.
- Most Providers businesses are online, Delta Dental's Provider Tools is online, so Providers wanted recredentialing online within their existing tools
- Other insurance companies offer online tools, Providers wanted it to be a Delta Dental standard as well.
- Anything that would reduce the amount of time being on the phone and on hold would allow Providers to spend more time with patients.
From these needs that were discovered through research, my team and I co-organized a design thinking workshop.
Workshop artifacts
The challenge
Knowing when it's due and what they have to do
We learned that:
Providers are unclear about when recredentialing is due, what they need to send and what Delta Dental already has, and feel stressed.
We wondered if:
Paper notifications and paper responses created a lot of ambiguity in the next steps.
A few issues that we needed to keep in mind were HIPPA privacy restraints and the types of information we could communicate in the email alert notifications.
Pain points included being a manual process, confusing timeline, lack of transparency about the process and lack of visibility on status.
Persona focused on - Esther, an Office Manager of a multiple offices practice, varying in size.
- Twelve years in an office with 4 Providers in the office contracting with Delta Dental.
- Deals with 8 different insurance companies.
- Desktop computers and tablets used in the office.
What Esther wants to accomplish
- Esther wants a better understanding of what to expect going into the process of recredentialing to be confident that they are doing it right the first time as to not waste time.
- She wants an easier way to be notified and remember the due date to plan ahead and not feel rushed.
- She wants to be able to complete the same 3-year cadence and the same time for all plans and locations to reduce redundancy.
- She wants to receive notification via preferred communication channel so they don’t miss it.
- Finally, she wants visibility into the stages and ability to check the status at anytime.
The solution
Recredentialing alerts
It would be ideal to proactively communicate with the Provider/Office notifying them of what is needed, what we already have and when it's due, communicating a trusted credentialing timeline that brings the Provider along with the process and supports a healthy, trusting relationship between Delta Dental, the Provider and patient.
Hypothesis
For Providers who need to stay in touch with their recredentialing, the digitized notification platform is a way to proactively alert Providers that need to update their information and maintain a transparent and trusting partnership.
Features
Digital notifications, in the form of alerts via email and in-app dashboard notifications.
Email alerts were designed to keep information communicated to a minimum to keep privacy at the forefront, only alerting to the name of the practice, the action needed, what Provider it was for and when it needed to be completed. Followed by a way (a clear link or button) in email to access the dashboard quickly.
Dashboard alerts offered more information for the practice and Provider. Including everything the email alert offered, added specifics of additional information that would be needed from the Provider, a call to action button to start completing the form, notification of other Providers at the practice’s next recredentialing due dates and a conceptual chat option for help.
Desired outcomes
- Transparency around recredentialing needs
- Ease of use for Providers
- Reduced processing cost
Desired results
- A reduction in open cases with missing information
- An improvement in Provider network accuracy
- A reduction in phone calls
- A reduction in mailing expenses
- Faster turn-around-time
Early wireframes & later interation mockups
The challenge
Back and forth after submitting
We learned that:
Providers find recredentialing feedback cumbersome and confusing with lots of ineffective mailings that leave them unsure if what they’ve submitted was done so successfully, and/or if there was wrong or missing information.
We wondered if:
Providers knew transparently what was missing and what was happening with their case and if that would limit their anxiety and concerns about coverage being dropped. Resulting in less calls and follow-up via telephone.
A few issues that we needed to keep in mind were HIPPA privacy restraints and the types of information we could communicate in the email alert notifications.
Hypothesis
For Office Managers who need to provide additional information for Providers within their office, a Provider credentialing dashboard provides push notifications to clearly display which information is required and the overall status of the recredentialing effort.
Pain points included being a manual process, confusing timeline, lack of transparency about the process lack of visibility on status.
Persona focused on - Millie, an Office Manager with 3 Providers in the practice.
- Has been working in the office for 3 years.
- Very busy office, works with 1 receptionist.
- Three Providers contracting with Delta.
- Deals with 4 different insurance companies.
- Uses a desktop computer and paper and pencil in the office.
What Millie wants to accomplish
- When submitting paperwork, Millie wants to get important updates as they occur in real-time so that she's not left wondering about the status of her paperwork and she can understand where she is in the process.
- When some time has passed after submitting her recredentialing paperwork, she want's to be able to look up her recredentialing status so that she's not left wondering where she is in the process.
- When she's looking at the credentialing status, she want to be able to quickly see the high level status of all of her Providers so that she know's where everyone is at in the process.
- When she's looking at the credentialing status, she want's to be able to dive into the details of each Provider so that she can easily understand exactly what to do to resolve any outstanding issues.
The solution
Email status updates and dashboard
It would be ideal to provide real-time status updates with details. Be able to share information appropriately with Providers based on their specific communication preferences. Giving them self-service tools to help them address issues/missing info. We could have an app!
Hypothesis
For Office Managers who need to provide additional information for Providers in within their office, a provider credentialing dashboard provides push notifications to clearly display which information is required and the overall status of the recredentialing effort.
Features
Digital status notifications, in the form of alerts via email and in-app dashboard notifications.
Email status notifications were designed to keep information communicated to a minimum and keep privacy at the forefront. Notifying with only the name of the practice and which Provider the status update pertained to. Followed by a general message that need the attention of the Provider or staff and when it needed to be viewed or completed by. Finally, it was followed by a way to access the dashboard quickly in the form of a link or call-to-action button to help view potential issues and/or fix any issues that could be remedied.
Dashboard alerts offered more information for the practice and Provider. Including everything the email alert offered with added specifics of actions or additional information that would be needed from the Provider. Also included was a call-to-action button to view the issue or fix the issue if it could be remedied. The dashboard also included viewable information of other Providers at the practice’s next recredentiling due dates and a conceptual chat option for help.
Desired outcomes
- Fewer calls to the call center asking about recredentieling status
- Increased transparency in timeline to reduce recredentialing turnaround time
- Increased provider satisfaction
- Reduced mailing costs due to status transparency on dashboard
- Reduction in provider terminations
Desired results
- An increased utilization of the Provider dashboard
- A reduction in recredentialing status inquiry calls
- Proactive usage of dashboard rather than reactive
Early wireframes
Later interation mockups
Setting up an Unmoderated Study in UserZoom
A collaboration case study for Product Designers working with UX Researchers
Planning your study and working with UXR
Working with UserZoom was tricky. Luckily, I had a great intro to the platform, and a great working partner with our Provider Experience User Researcher. Together, we were able to get the Claims Submission study off the ground.
Setting up a study
Partner with UXR early
As a designer, I would recommend partnering with UXR early and communicate what you want to learn from setting up a study and leave ample time for recruiting.
For this study we wanted to know:
- How Providers typically submit claims
- How Providers typically attach files and if file attachment accordion was discoverable
- Whether the new layout was clearer and easier to scan than previous layout
- If the list of claims table was after claim was submitted, was easy to understand
Planning and working with a UXR
- Communicate what you want to learn (your goals) from the study, and who you think should be a part of the study (personas).
- From there you should be able to determine:
- The type of test needed
- Prototype needs
- Direction for recruiting participants
Get to know UserZoom test options
- Logging into UserZoom for the first time can be daunting, but you can do this!
- In this case, you will choose an Unmoderated Study.
- An Advanced UX Research study was used for the Claims Submission study, but check with UXR and see which is right for you.
- The Claims Submission test included a questionnaire, 3 separate tasks to test the designs and a follow-up questionnaire. We set the study up to record the participant from start to finish.
- UserZoom videos are helpful, but not as helpful as actually starting to craft questions in UserZoom.
UserZoom process for setting up a study
Working with Sketch
Prepping the prototype for testing
- I needed more screens with more states to test than I needed to communicate the designs with stakeholders.
- We eliminated 1 version based on the discovery with Product Managers and based on the purpose of the study.
Using Craft plugin + Sketch prototyping = headache
Work in Sketch to build your prototypes and link them using the Craft plugin to build out different versions to test.
I recommend using either the Craft plugin to create links, or Sketch prototyping, but not both. It’s easier to troubleshoot if using only one source of hotspot linking.
You may need to create more than one project in InVision if you are testing more than one flow.
Working with InVision
Share Prototype settings
Make sure you have Hotspots enabled and Prevent hotspot hinting as the only options turned on.
You can access the additional settings in Share -> Link Settings -> More Options.
Sketch & InVision learnings
- Only use the craft plugin for assembling the links
- I found that with troubleshooting, only using 1 source (as opposed to using Sketch prototyping) is better for eliminating errors.
- My test kept linking to the wrong page, I wasn’t sure where the source of the error was since I was using both Sketch and Craft.
- I removed all native Sketch prototyping links to troubleshoot and eliminate culprits.
- Time consuming
- Share links in InVision:
- Use the share link in InVision, not the link to the prototype.
- Sounds obvious, but I made the error of using the wrong link.
- Sometime’s UserZoom links to the wrong page in the prototype, to eliminate this, try designating the first screen of the prototype in InVision.
Working with UserZoom
Setting up your prototype tasks
There are a variety of different ways to set up an unmoderated test with potentially several different question types and URLs for each task:
- Intercept URLs
- Success URLs
- Validation URLs
You’ll want to make a note of all the URLs that will be part of the test.
Follow-up questions are crucial
- Use visual references to ask specific follow up questions as needed:
- You may need to use a static image.
- Test and make sure the image has the right resolution and size (I exported @0.5 from Sketch).
- Annotate the image so that you are calling out the area in question and make it clear for the user.
UZ process for setting up tasks and questions
UserZoom Task Management
UZ Questionnaire Types
UserZoom Question Options
Pilot test and monitor!
Allow plenty of time to test and iterate, I learned the hard way
- Allow for enough time to test.
- I went though the test preview many times and had to find/fix errors, and continued to and tweak and optimize questions.
- The first couple of participants act as QA.
- After watching a couple of the videos, we found errors, had to pause the test, make changes and relaunch.
Final thought...
Despite the challenges, learning UserZoom was worth it.
My recommendation would be to start with a small study and run through the process.